Medical professionals can discern a great deal of information from the pupillary light reflex. For example, each pupil’s size can indicate whether a person has a traumatic brain injury.
Pupillary evaluation is also used to evaluate conditions affecting the brain, such as strokes and brain tumors.
But what is the significance of different pupil sizes for the evaluation of pupillary reaction? This article will explore the implications of each size and what it means for the patient’s health.
Is it expected to have pupils of different sizes?
The pupils of both should dilate equally in response to light. If they don’t, it can signal something wrong with the eye or nervous system. A neurologist may perform a pupillary evaluation to determine whether a patient has anisocoria or damage to their optic nerve, which carries visual information from the eyes to the brain.
When is anisocoria normal?
There are three types of anisocoria: normal, physiologic, and pathologic.
Normal anisocoria is when one pupil is larger than the other, but both pupils normally react to light. It’s common in young children and usually resolves as they get older.
Physiologic anisocoria occurs when there is a difference in pupil size due to accommodation. This means that one pupil is dilated while the other is constricted.
Pathologic anisocoria is when one pupil is larger than the other, and both pupils do not normally react to light. This can be a symptom of an underlying medical condition, such as inflammation or traumatic brain injury.
How can the doctor determine whether anisocoria is because of an underlying medical problem?
A pupillary evaluation can help the doctor determine whether anisocoria is due to an underlying medical problem. This exam may include a visual acuity test and a neurologic evaluation.
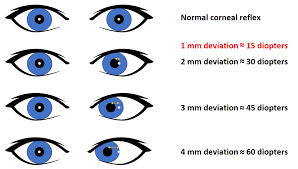
The doctor will measure the size of each pupil in both eyes using a light reflex test or a handheld device called a pupilometer.
A pupilometer helps measure pupil reactivity to light. The doctor will also assess the visual field, the area covered by both eyes when looking straight ahead. If the patient’s vision and anisocoria are impaired, this condition may be due to a retinal problem or brain injury.
How does the doctor know if the big pupil is “too big” or the small pupil is “too small”?
Assessing anisocoria requires knowing which pupil has a larger pupillary distance. When light levels drop, pupils dilate; if the miotic pupil isn’t widening as it should, something may be amiss. The non-contraction of the larger (mydriatic) pupil in bright light may be abnormal (or growing smaller).
What causes an abnormally large (dilated or mydriatic) pupil?
After an eye injury, if the iris tissue is damaged, it is possible that the pupil may not normally respond to bright light and will remain open (i.e., a concussion). Adie’s tonic pupil syndrome may also be involved.
The disease often manifests itself in one eye first, and young adult women are disproportionately affected. Pupils are notoriously slow to react to light. Many patients with this condition also have decreased deep tendon reflexes, making it difficult to focus on details at close range.
In most situations, the disease is not associated with severe health issues. Eye drops, nasal sprays, and other medications may all be used to dilate the pupil. Ant antiperspirant wipes intended for another purpose might cause temporary pupil dilation if put into the eye.
Finally, a pupil abnormality might result from a problem with the third cranial nerve, which connects the brain and the eye. Pupil dilation and lid movement are within the third cranial nerve jurisdiction. Drooping of the upper eyelid, or Ptosis is a frequent symptom of this condition, as is a dilated pupil.
An older child may also complain of double vision since the eye is not moving as it should. In patients with third cranial nerve palsy, the doctor may want to order urgent brain imaging studies to rule out more serious concerns.
What are some causes of an abnormally small (miotic) pupil?
There are several causes of a miotic pupil. The most common is Horner’s syndrome, caused by damage to the sympathetic nerve fibers that travel from the spine to the eye.
What are the signs of Horner’s syndrome?
Horner’s syndrome causes a drooping eyelid, a smaller pupil, and an inability to widen the eye with lenses. The pupil may also be irregular or shaped.